Grand Rounds at University of Washington. Discussing the importance of recognizing vascular injuries in the setting of knee trauma and the devastating limb-threatening consequences of missed vascular injuries.
Dr. Nels E. Sampatacos, surgery resident with UW Medicine, begins the lecture with a case study along with functional anatomy concepts.
Dr. Benjamin W. Starnes, chief of vascular surgery for UW Medicine, shares his personal military experience as a vascular surgeon, providing unique insight into front-line management protocols.
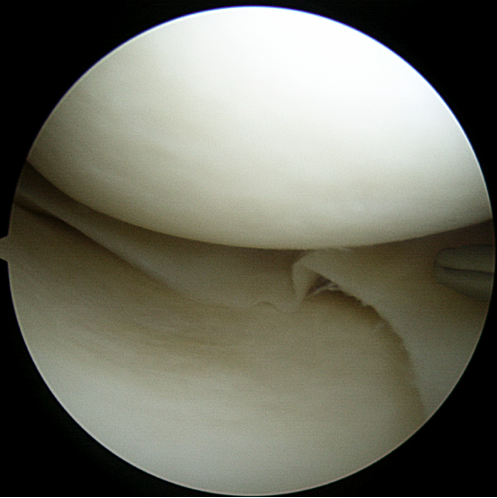
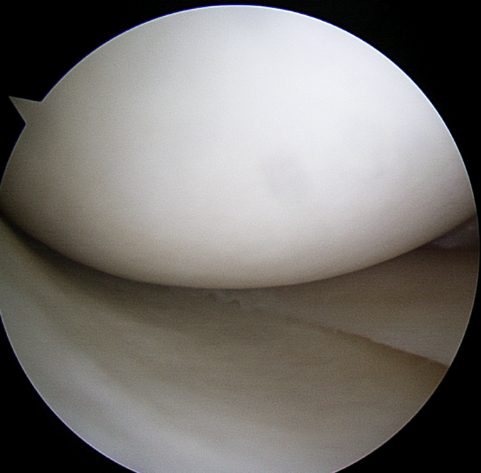
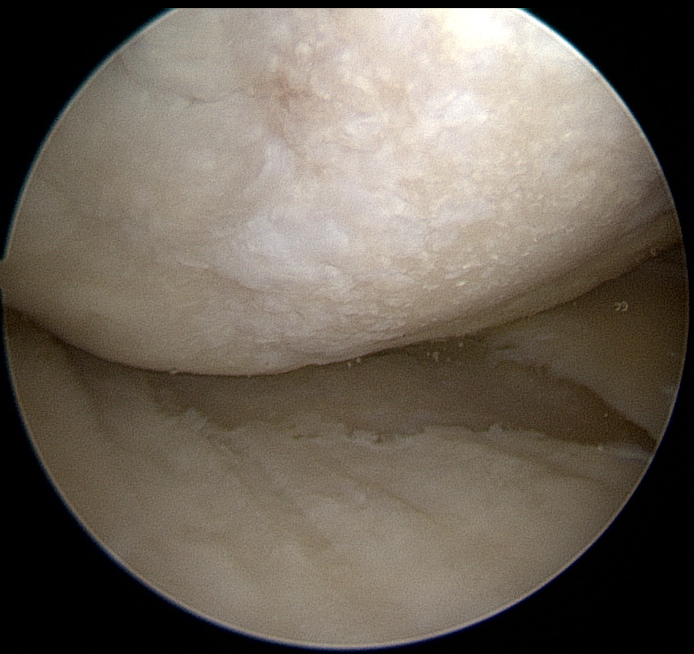
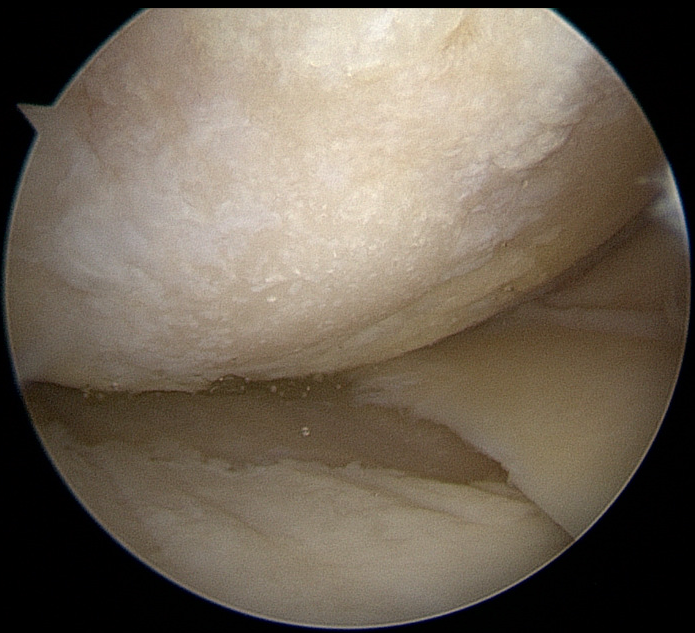
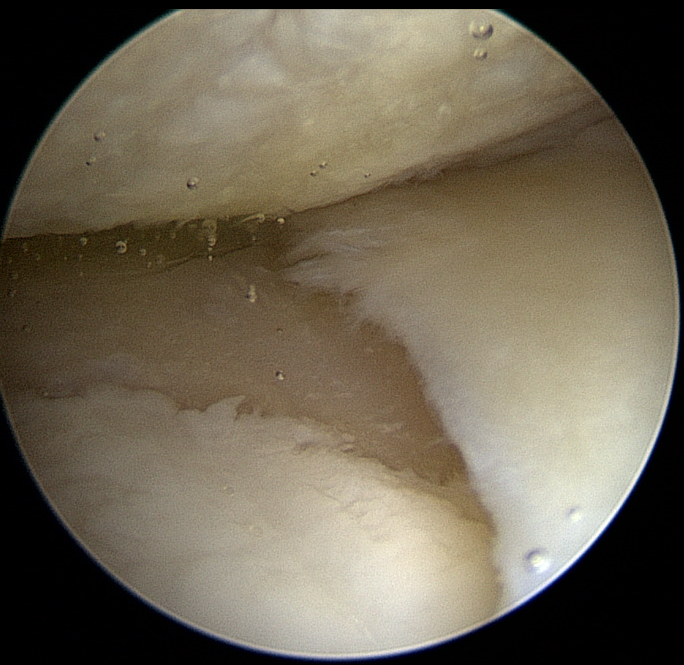
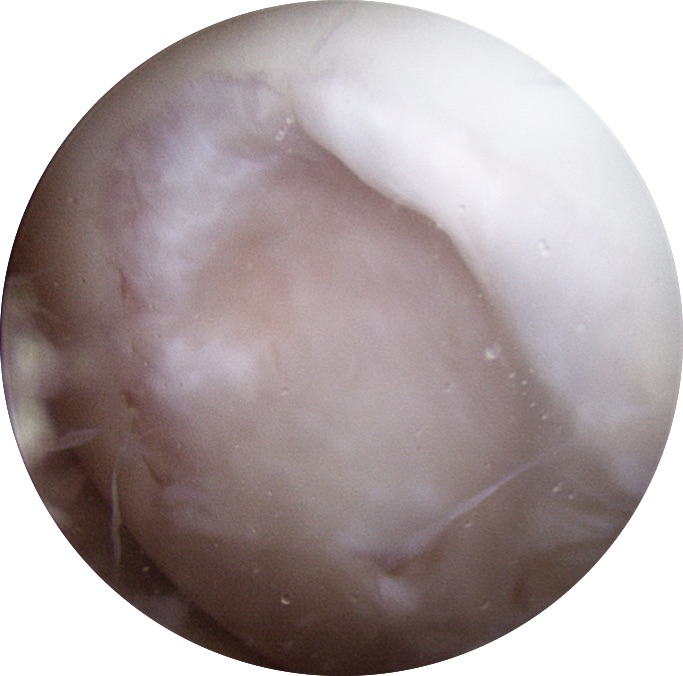
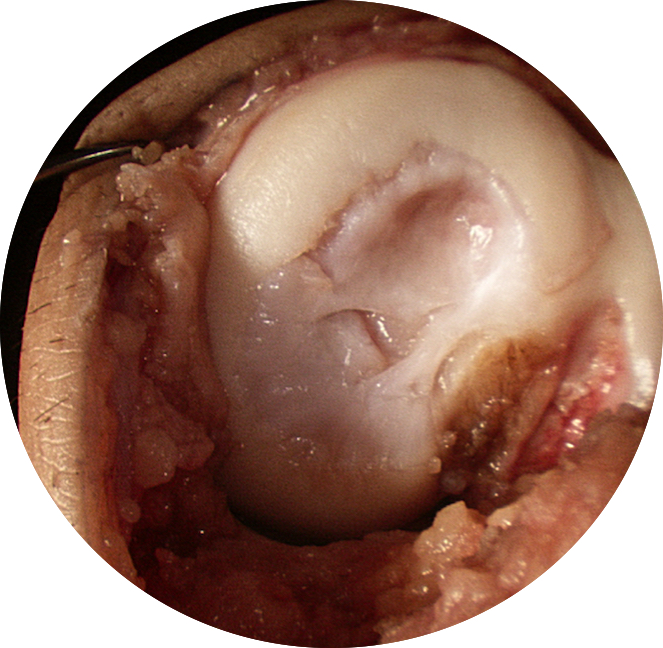
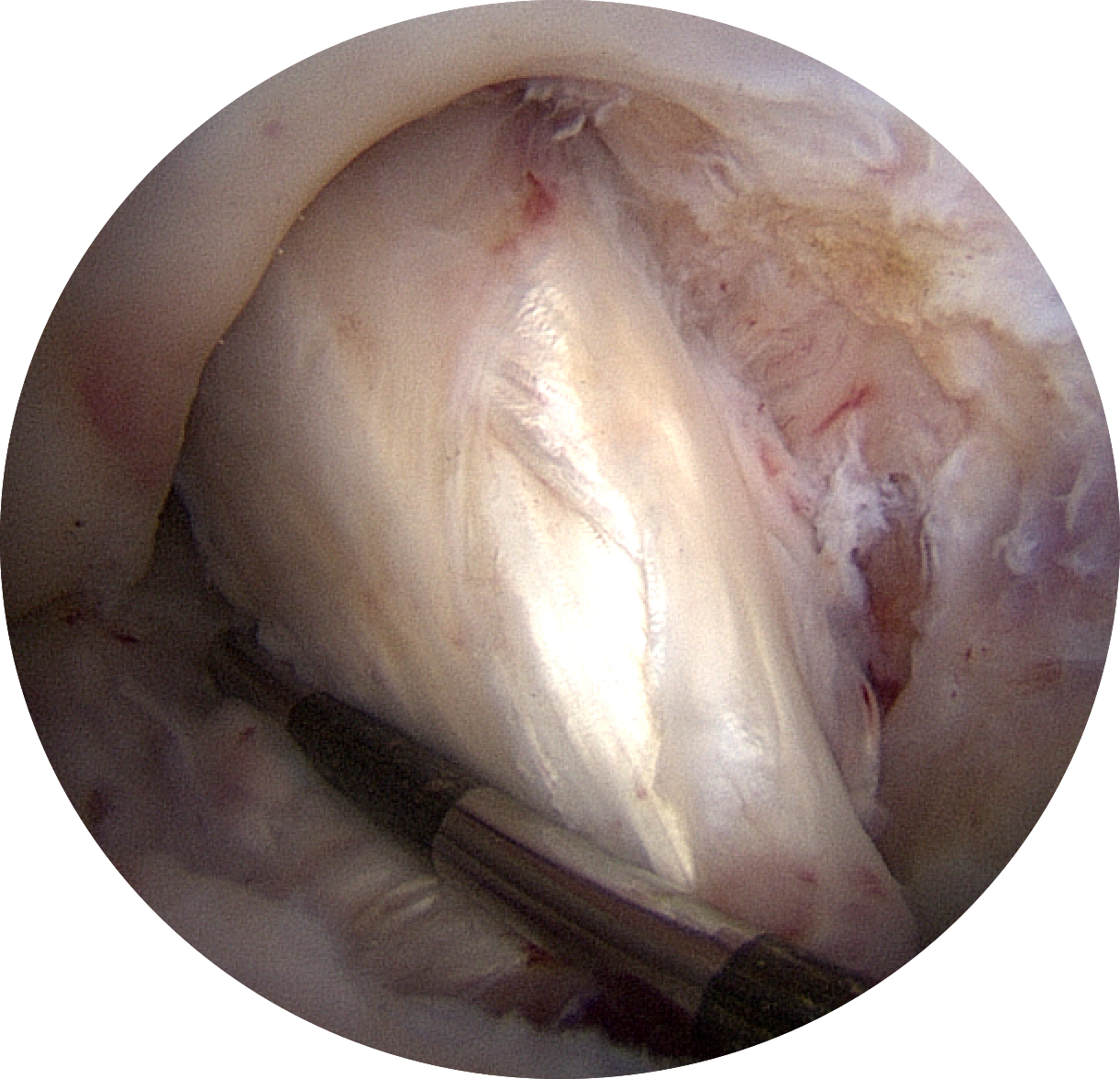
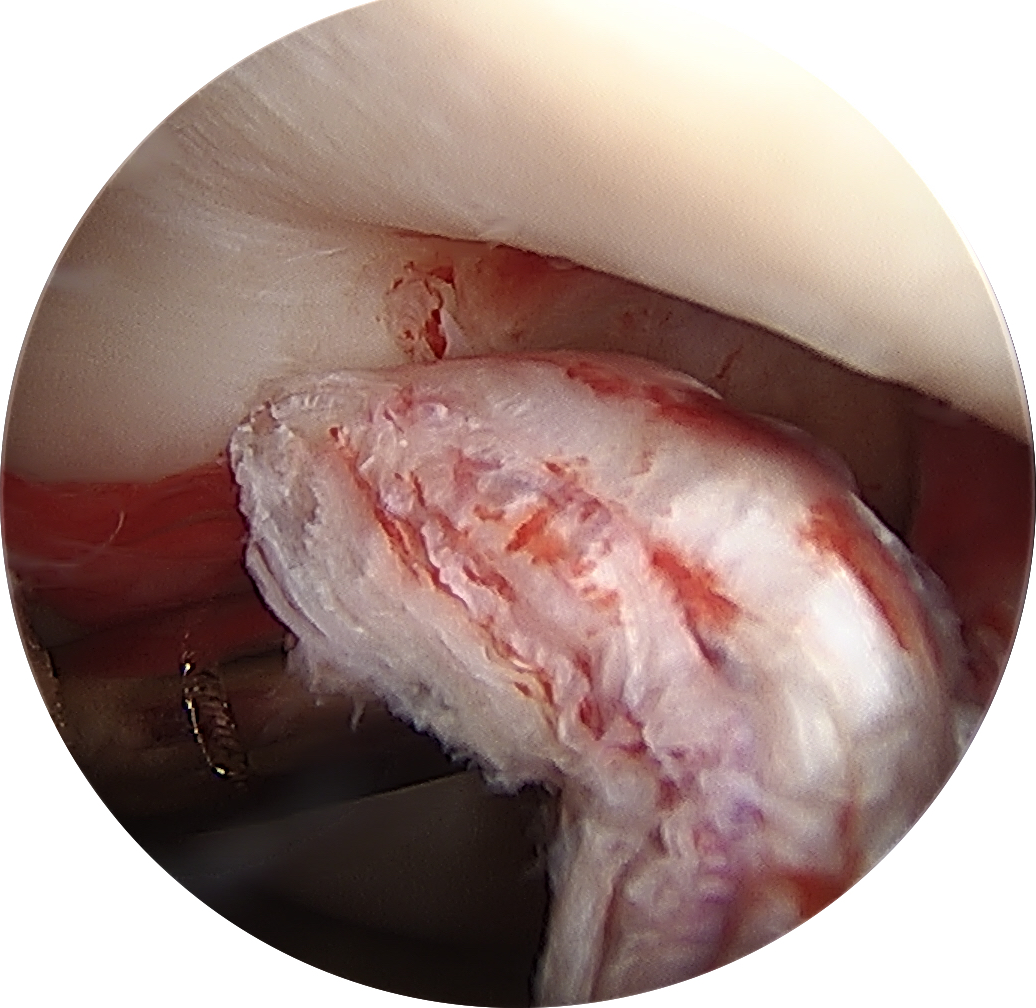
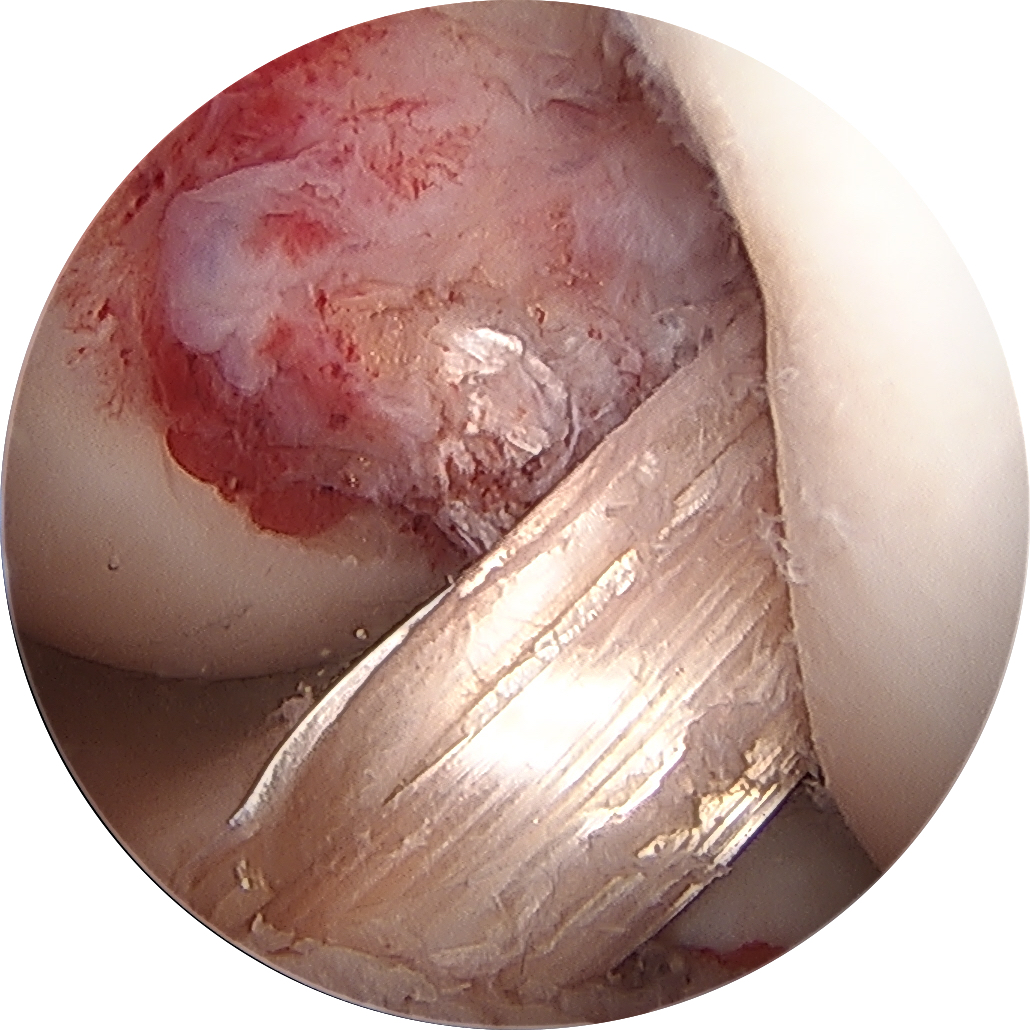
Dr. Christopher J. Wahl, assistant professor with the University of Washington, discusses orthopaedic perils and pitfalls, focusing on the radiographic findings suggestive of vascular injury in the setting of knee dislocation.